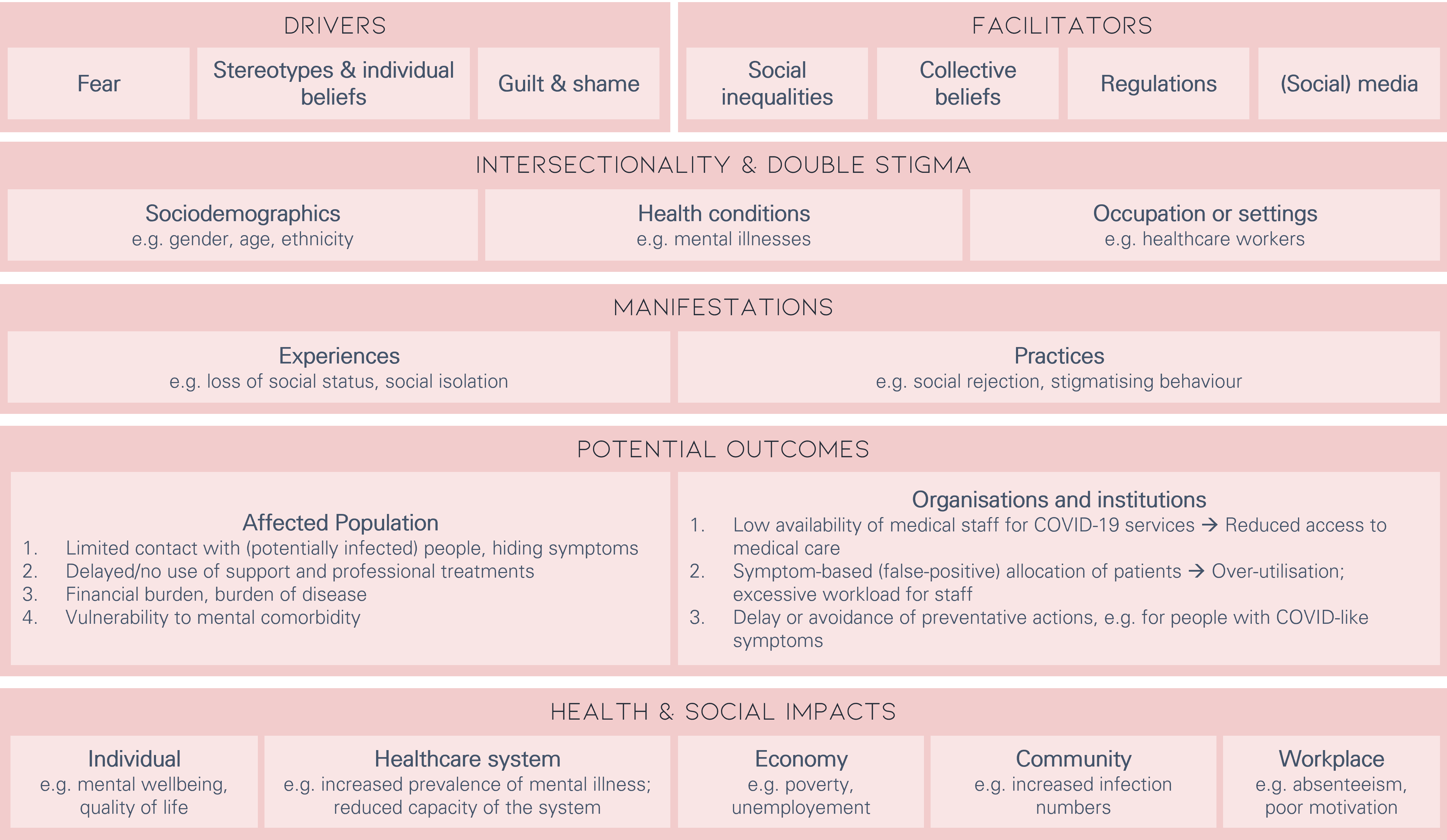
Health Stigma and Discrimination Framework
The StiPEx project utilizes the Health stigma and Discrimination Framework (HSDF) (Stangl et al. 2019) that was adapted to the context of the COVID-19 pandemic (Ransing et al. 2020).
Drivers and facilitators but also Intersectionality and Double Stigma determine the occurrence of stigmatisation and the way in which the affected persons are being stigmatised.
Reinforcing factors
Reinforcing factors include drivers and facilitators as well as Intersectionality and Double Stigma.
Drivers
Individual factors that determine the occurence of "marking" as a prerequisite of stigmatisation . Drivers are generally negative, and include:
- fear
- stereotypes and individual beliefs
- guilt and shame
facilitators
External factors can also have an impact and can be perceived as negative or positive. These include:
- social inequalities
- collective beliefs
- regulations
- (social) media
Intersectionality & Double Stigma
Factors that facilitate or intensify stigmatisation. Intersectionality occurs when a person is labelled with multiple stigmatised attitudes. This can involve aspects such as:
- sociodemographics
e.g., gender, age, ethnicity - health conditions
e.g., mental illnesses - occupation or settings
e.g., healthcare workers
Manifestations
People who experience or observe stigmatisation often act differently from others. Some people even stigmatise themselves because of their experiences.
Experiences
e.g., loss of status, social isolation
Practices
e.g., social rejection, discrimination
Potential outcomes
Taken together the above mentioned factors can have a negative impact on the level of the affected populations as well as on an organizational level.
Affected population
- Limited contact with (potentially infected) people; concealment of symptoms
- Delayed/no use of support and professional treatments
- Financial burden; increasing burden of disease
- Vulnerability to comorbid mental illness
Organisations and institutions
- Low availability of medical staff for COVID-19 services → Reduced access to medical care
- Symptom-based (false-positive) allocation of patients → Over-utilisation; excessive workload for staff
- Delay or avoidance of preventative actions
Health & social Impacts
In the long term, stigmatisation has an impact on various areas:
- Individual
e.g., mental wellbeing, quality of life - Healthcare system
e.g., increased prevalence of mental illness, reduced capacity of the system - Economy
e.g., poverty, unemployement - Community
e.g., increase in infections - Workplace
e.g., absenteeism, poor motivation
Literature
Ransing, R., Ramalho, R., de Filippis, R., Ojeahere, M. I., Karaliuniene, R., Orsolini, L., . . . Bytyçi, D. G. (2020). Infectious disease outbreak related stigma and discrimination during the COVID-19 pandemic: drivers, facilitators, manifestations, and outcomes across the world. Brain, Behavior, and Immunity.
Stangl, A. L., Earnshaw, V. A., Logie, C. H., van Brakel, W., Simbayi, L. C., Barré, I., & Dovidio, J. F. (2019). The health stigma and discrimination framework: a global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Medicine, 17(1), 1-13.

